Diagnostics
Reflux—GERD—Heartburn
The clarification of the reflux disease—GERD is carried out on the one hand morphologically 2 with a gastroscopy (gastroscopy). With this examination, in addition to assessing the duodenum and stomach, a diaphragmatic hernia (hiatal hernia) and esophagitis can be diagnosed, usually on the basis of reflux disease.
It is also possible to determine the position and height of the mucosal boundary between the stomach and the esophagus, to exclude a CLE (columnar lined esophagus) and a potentially pathological change in the mucous membrane - the cardiac mucosa (CM), which subsequently becomes Barrett's mucosa (intestinal metaplasia; IM) can develop, diagnosed by multilevel biopsies (tissue samples). The new technology of narrow band imaging (NBI), which, together with chromoendoscopy, achieves a very good and significant improvement in the visibility of the tissue structures and thus enables the pathologies to be identified more easily and earlier, has a contrast-enhancing and thus diagnostic support. The early detection of the reflux-based mucosal changes in the direction of Barrett's is absolutely essential, so that a rapid, adequate therapy of reflux GERD can be initiated and further damage to the esophagus and thus transformation into an esophageal carcinoma (esophageal cancer) can be avoided.
In order to get an impression of the extent to which the esophagus is actually exposed to aggressive substances, a quantitative 2 examination is added and the question of what, how much, how often and under what circumstances flows back from the stomach into the esophagus, answered.
The 24-hour impedance measurement has almost completely replaced pH metry, has a very high specificity and good sensitivity and for the first time you can make a good statement about the strain on the esophagus. In addition to the qualitative and quantitative recording of the reflux, a symptom correlation can also be carried out. This correlation is very important, especially in the case of symptoms that are not quite typical for reflux, whether the symptoms felt are reflux-associated or not. Both statements are essential, because if there is a high correlation, a therapy that restricts the reflux will to a large extent not only make the reflux itself disappear, but also the symptoms. To a certain extent, the symptom correlation represents a predictive factor as to which treatment will improve or completely treat the symptoms and /or reflux. The measurement takes place on an outpatient basis either in my ordination in the 1st district or in Reflux Center of the Döbling Private Clinic .
In the case of special questions, especially in the presence of reflux GERD despite the morphologically intact closure mechanism between the stomach and esophagus, suspected esophageal motility disorder (esophageal movement disorder) or achalasia, a manometry is performed. It is an outpatient examination in which the various pressure levels in the esophagus are measured depending on the time axis and thus allows conclusions to be drawn about the competence of the sphincter between the stomach and esophagus and an assessment of the esophageal movement. So-called transient relaxations (spontaneous relaxation) of the lower esophageal obstruction are also recorded well with this measurement and are incorporated into the decision-making process as to which type of therapy will be the most promising. The impedance measurement is usually carried out together with the manometry (HR impedance manometry).
Finally, with functional diagnostics 2 , the Videokinematographie , radiologically the situation assessed dynamically. A reflux GERD can actually be visualized and the size of a diaphragmatic hernia can be correlated again with the gastroscopic findings. In addition to evaluating the sequences of the transport of a bite through the esophagus, detecting a movement disorder and assessing the ability of the esophagus to empty, the HIS angle (angle between the axis of the stomach and the axis of the esophagus) can also be determined. This becomes blunt when the occlusion device between the stomach and esophagus (cardia, lower esophageal sphincter - LES) slides in the direction of the chest due to the stomach ligament that has become too weak. This phenomenon occurs with an axially sliding diaphragmatic hernia (axially sliding hiatal hernia) and usually occurs with larger or relevant diaphragmatic hernias.
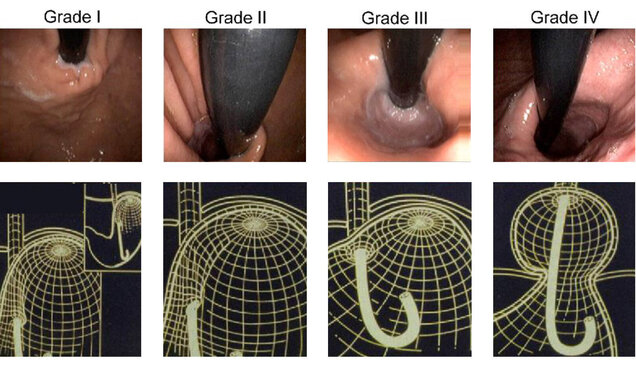
The diaphragmatic hernias are classified according to Hill . The final ability is displayed and assessed in three dimensions.
Further information on the topic
Impedance measurement
The impedance measurement is one of the most modern methods for a quantitative clarification of the reflux disease and is clearly superior to conventional pH metry in terms of information content.