Diseases of the esophagus
The esophagus (Latin: Ösophagus) is a hollow organ and connects the throat with the stomach. Their job is to convey the food, which has been mechanically chopped in the mouth, into the stomach. The esophagus has several muscle layers that are controlled by an independent nerve network that sits directly in the wall. The movement of the esophagus is therefore automatic and is not subject to arbitrariness.
Functional disorders
There are numerous movement disorders of the esophagus (esophageal motility disorder), which occur primarily or as a result of other diseases and are very unpleasant: e.g. jackhammer esophagus, nutcracker esophagus, esophageal spasms. The main symptoms for this include the feeling that a bite is stuck (dysphagia), pain and cramps behind the breastbone, globus feeling (dumplings in the throat), vomiting, and much more The main cause of esophagitis is the rare eosinophilic esophagitis (EoE), constrictions (inflammatory, systemic disease or tumorous), a Schatzkiring or a primary or secondary expansion of the esophagus, such as achalasia, can be the cause of a movement disorder. In any case, a thorough clarification makes sense, because the earlier an esophageal disease is detected, the easier it is to treat it. This also applies to the treatment of tumors in the esophagus. If an esophageal carcinoma is detected early, this tumor disease can also be treated very well.
The gastroesophageal reflux (GERD, reflux oesophagitis) as the most common disease of the esophagus is treated separately.
Achalasia
Achalasia is a rare neurodegenerative disease of the esophagus with a frequency of 1-3 /100,000 cases per year and a peak between 20 and 40 years of age. Age. Achalasia is the lack of or insufficient swallowing-induced relaxation of the lower occlusive apparatus between the stomach and esophagus (lower esophageal sphincter or LES). That sounds more complicated than it is. Under normal circumstances, a bite that has been crushed in the mouth and then swallowed triggers a so-called coordinated peristalsis wave, which transports the food from the throat towards the stomach, and an opening of the lower esophageal sphincter at the beginning of the swallowing process. If this opening does not take place or is insufficient, the food cannot or not completely enter the stomach and some of it remains in the esophagus. In the best case scenario, this part can be conveyed by swallowing it into the stomach or by drinking afterwards. If that doesn't work, vomiting or regurgitation occurs. In the worst case, a piece that can no longer be mobilized has to be removed by the doctor.
Achalasia has different causes, can occur primarily in the context of a systemic disease or, significantly more frequently, secondary /functional in the context of a reflux disease that has existed for years and has not been adequately diagnosed or inadequately treated in the case of peptic stenosis. Achalasia can also develop after an operation on the esophagus (iatrogenic achalasia). Depending on the severity of the pathology and how long the disease has existed, a secondary movement disorder of the esophagus occurs, followed by an expansion and finally a complete standstill of the peristalsis. In this state it is almost impossible to eat. The main symptom is swallowing disorder (dysphagia), but regurgitation (backflow of undigested food) can be the first symptom in up to 40% of cases.
Diagnostics are based on precise medical history, gastroscopy, manometry and video cinematography
The therapy takes place via stretching in the course of a gastroscopy, via botox injections of the LES in the initial stage, via an endoscopic procedure in which the spinal muscle fibers are split over a long distance into the upper part of the stomach (so-called POEM: peroral endoscopic myotomy) or surgically . In the latter technique, called laparoscopic cardiomyotomy according to Heller, the sphincter muscle fibers of the upper part of the stomach are split in a minimally invasive manner up to about 10 cm of the lower esophagus.
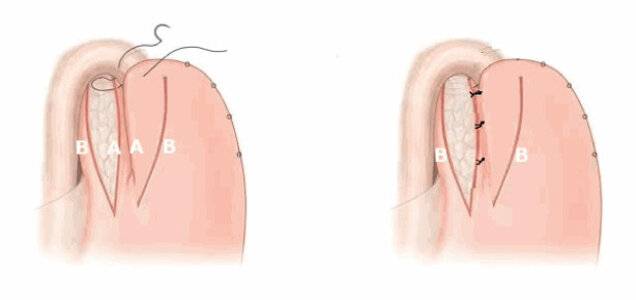
The defect is covered with a Toupet fundoplication (posterior 270 degree cuff) or better with an anterior hemifundoplication according to Dor. In this way, a reflux component that often exists simultaneously is also treated at the same time.
The most effective is surgery. The quality of life can be significantly improved in the long term. After a short phase of diet, the patients can generally leave the hospital after 2-3 days and lead a completely normal life.
Other diseases such as diverticula of the esophagus (Zenker's diverticulum, epiphrenic diverticulum, ...) or Schatzkiring are rare.
Benign tumors
Are rare and there are a number of different entities. In most cases, however, it is a matter of leiomyomas. Much more common are malignant esophageal tumors (malignant esophageal carcinoma).
Esophageal cancer - esophageal cancer - squamous cell carcinoma
Esophageal carcinoma (malignant tumor of the esophagus) is a rare disease. Men over the age of 55 are most frequently affected. On the basis of the fine tissue (histological) picture, a distinction is made between two different forms: the increasingly rare squamous cell carcinoma - mostly located in the upper 2/3 of the esophagus, and the adenocarcinoma, which is clearly increasing in frequency - mostly located in the lower third.
The main causes of squamous cell carcinoma are high-fat foods as well as low-protein and low-calorie foods. Very hot food or drinks, alcohol consumption, the influence of nitrosamines and smoking are also established risk factors for this type of cancer.
Barrett, Barrett's esophagus, Barrett's carcinoma
For adenocarcinoma is not or inadequately treated gastroesopahgeal reflux (GERD - acidic and bilious stomach contents flowing back into the esophagus) responsible . With reflux that has existed for years, chronic damage to the esophageal mucosa can lead to cell changes at the transition from the gastric mucosa to the esophageal mucosa after different periods of time. A precancerous stage (precancerosis) develops, the so-called Barrett's esophagus. The Barrett's esophagus without dysplasia develops after years of low and high grade dysplasia into an esophageal carcinoma (esophageal cancer). From a statistical point of view, this process is analogous to the development of a polyp (adenoma) in the intestine in colorectal cancer (colon cancer). The times are different, with the most recent publications in the specialist literature giving the time of development of a malignant esophageal tumor from a Barrett's without dysplasia as 3 years 1 . It is therefore essential to adequately and adequately treat reflux as the causative cause of Barrett's and Barrett's esophagus. Depending on the stage of dysplasia, local procedures with destruction of the Barrett's (radiofrequency ablation) or more modern with resection of the Barrett's mucous membrane are endoscopic (EMR - endoscopic mucosal resection) or, in more advanced stages, ESD (endoscopic submucosal dissection) or surgical (partial) removal of the Carry out esophageal resection.
Untreated or insufficiently treated (mixed) Reflux is the strongest risk factor for esophageal cancer !
The association between reflux, Barrett's and higher mortality rates compared to the non-reflux population is summarized in this study: